TFCC tears / DRUJ instability
Anatomy
The distal radio-ulnar joint (DRUJ) is the joint between the lower end of the radius and the ulna. It is part of the forearm, whose motion allows the hand to be placed palm down, palm up and everything in between.
At the distal radio-ulna joint, the radius is gently concave and the ulna head gently convex (see figure).
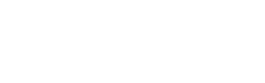
Because the joint surfaces are relatively flat, the joint relies on ligaments to keep the surfaces together. The most important of these ligaments are the radio-ulna ligaments, there are two, the volar (palm side) and dorsal (back of hand side) , see figure. The volar is attached to the volar lip of the radius, at the edge of the DRUJ and the dorsal from the dorsal edge. They converge towards the ulna, at its pointy part (the styloid) and at a pit at the base of the styloid, the fovea. Thus they make a shape close to a triangle (see figure).
The area between the ligaments is normally filled by a sheet of fibrocartilage (shiny white stuff). This whole structure is has the somewhat complicated name – the triangular fibrocartilaginous complex (TFCC).
The TFCC is really part of the forearm, as well as part of the wrist.
TFCC/DRUJ problems
There are three common patterns of problems around the DRUJ/TFCC:
1. Tears of the TFCC with a stable DRUJ:
In this problem there is a tear of the TFCC which does not lead to deficiency of the dorsal and volar radio-ulnar ligaments. From the patients point of view, this means pain, but no clunking. From the surgeon’s point of view, this means that there is no abnormal motion of the DRUJ when it is stressed on examination.
Sometimes these tears can heal without surgery. If the pain is ongoing, then an arthroscopic suture repair may be helpful in promoting healing.
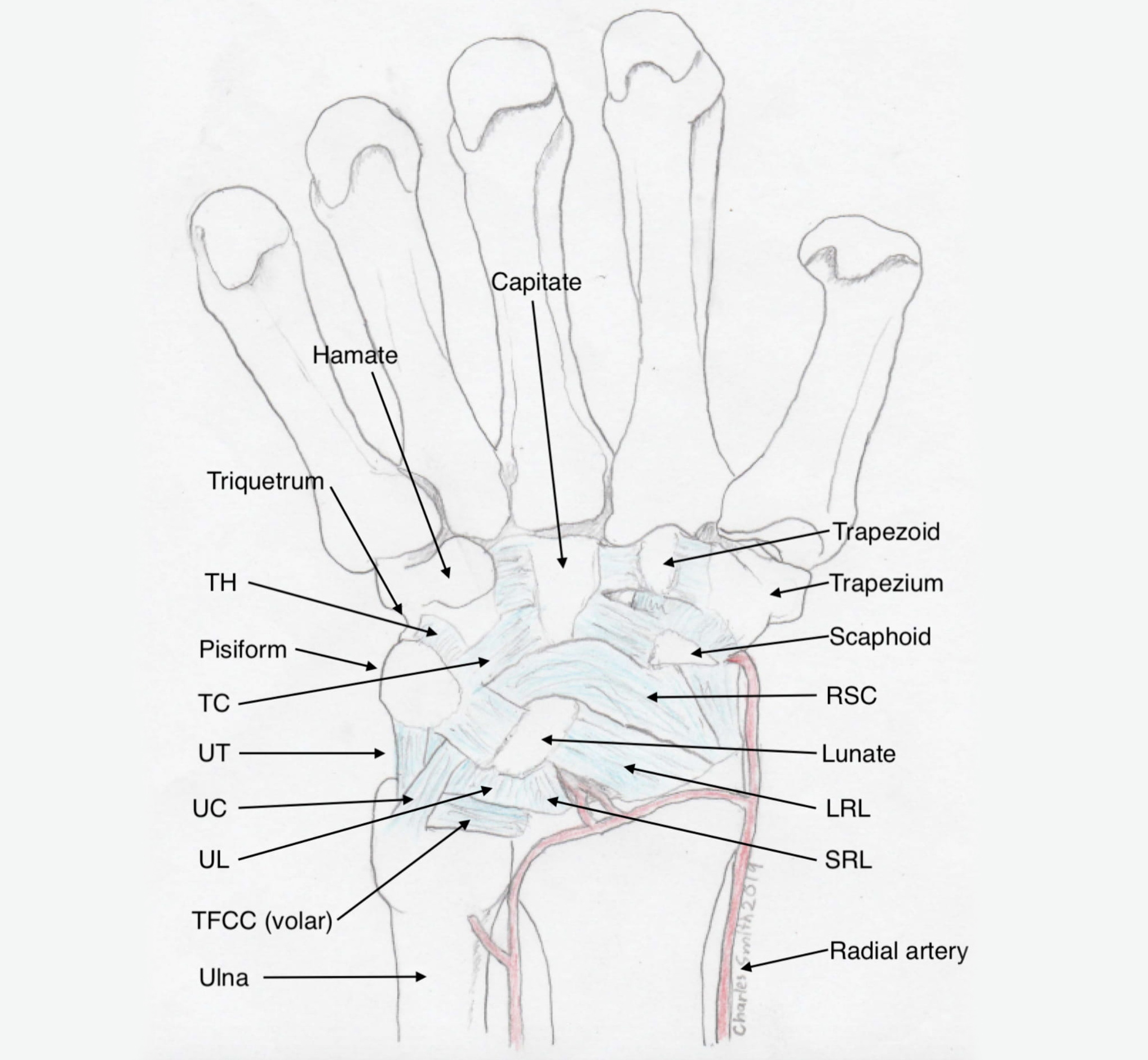
Top: volar wrist ligaments, Bottom: dorsal wrist ligaments

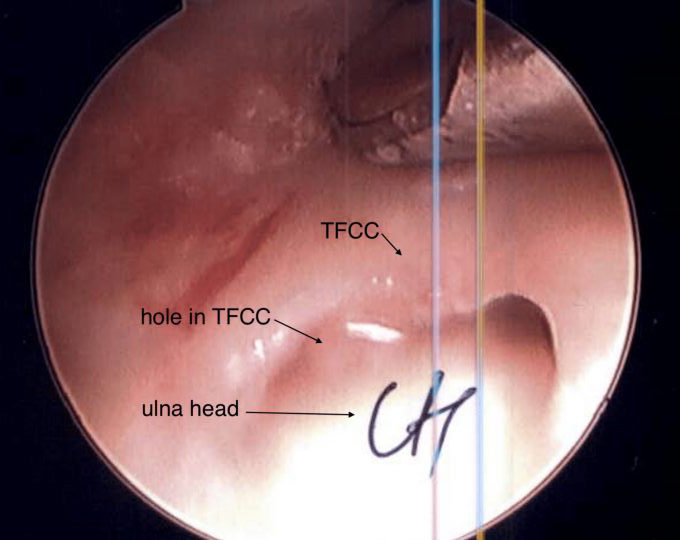


Top: X-ray of ulno-carpal abutment, where the ulna is too long. The situation has led to a cyst forming in the lunate, the central bone in the first row of the wrist, Middle: arthroscopic view of the TFCC defect in ulno-carpal abutment. The head of the ulna is visible through the defect. Bottom: X-rays following an ulna shortening osteotomy. Here an exact thickness of bone is excised from the ulna, and the bone ends are compressed and held together with a plate and screws.
2. Tears of the TFCC with an unstable DRUJ:
When the tear of the TFCC completely disrupts either the volar, dorsal or both the radio-ulnar ligaments, then there is abnormal motion between the radius and ulna (instability). From the patient’s point of view, this may lead to clunking at the joint with forearm motion (turning the palm up and down). From the surgeon’s point of view, this means that abnormal motion occurs between the two bones with stressing the joint. Tears like these can also lead to abnormal motion of the extensor carpi ulnaris tendon, which is restrained by a ligamentous hoop which is connected to the ulna by part of the TFCC.
These tears are less likely to heal without surgery. An accurate arthroscopic evaluation is very important in determining what is torn and where. This will allow the surgeon to plan an effective repair or reconstruction. If the TFCC has been pulled off the radius, then a reconstruction may be more effective than a repair. This means making new dorsal and volar ligaments, using a tendon graft through bone tunnels. If the TFCC has been pulled off the ulna, then a mini open repair can lead to a fairly predictable good result.
3. Ulno-carpal abutment:
Normally the ends of the ulna and radius are the same lengths at the wrist joint. There is individual variation though, and in individuals where the ulna is longer than the radius, the end of the ulna can butt its way through the TFCC over time, damaging itself, and also its neighbour in the wrist, the lunate. Sometimes this pattern of injury can occur relatively acutely, that is following a single injury.
The relative length of the ulna to the radius can only be accurately determined with standardised x-rays (variance or 90/90 views).
When this condition is present, and symptoms won’t settle, then the most effective surgical treatment is an arthroscopic debridement (clean up) of the shredded TFCC and an operation to shorten the ulna (ulna shortening osteotomy) – see figure.
After arthroscopic debridement alone, the symptoms will persist in about 50%. With ulna shortening, the underlying problem is corrected, and a more permanent improvement in symptoms generally follows. To shorten the ulna, the bone is approached through a 12cm skin incision, and using a special guide, an exact amount of bone is removed using two parallel cuts. The intervening fragment is removed, the two bone ends are compressed together and stabilised with a plate and screws. The bone normally takes around three months to completely heal. Usually the wrist symptoms are improved by about 1-2 months,
before the bone has completely healed. Whilst this sounds like a lot to do, it is not as painful as it sounds, as the bone is immediately firmly stabilised by the plate.
The plate can lead to ongoing local irritation, and around 50% of patients will request the plate be removed, if they are offered this option. Fortunately, this is a relatively simple surgery, with a rapid recovery.
4. DRUJ arthritis:
When the cartilage surfaces of the DRUJ are worn out or damaged, then pain may arise from the uncovered bony surfaces rubbing on each other.
Depending on the age of the patient, the underlying cause and the degree of symptoms, various surgical options may help. Although there is no perfect surgical solution, many patients do benefit from well considered procedures. However, I usually recommend that patients with this problem use non-surgical options for as long as they can.
The main surgical options are:
1. Darrach procedure – or excision of the ulna head. After this there is really no DRUJ, and improvements in pain may deteriorate if the patient is active.
2. Sauvé-Kapandji procedure – the radius is fused to the ulna through the DRUJ, and a segment of ulna is excised, to allow motion to occur through a gap in the ulna. Whilst this can help a lot in some patients, there can be problems in high demand patients.
3. Watson procedure – the joint surface of the ulna is excised and a tendon or muscle placed between the radius and ulna to act as a buffer. This works quite well in lower demand patients, especially after distal radius fractures that have healed in abnormal alignment, in patients with this bone, where realigning the radius might not work.
4. Ulna head replacement – this is a “half” joint replacement, made from metal or pyrocarbon. It can give good relief of symptoms, but is a joint replacement, and therefore does not last forever!
5. Constrained DRUJ replacement – this has gained popularity recently. It can give spectacular early results, but again is subject to later failure, like all joint replacements.